The interest in ‘endocrine’ glands began in antiquity when the most obvious organs accessible to the knife, the testes, were sometimes removed either to make the harem safe, or to extend the duration of the male soprano voice into adulthood. On a culinary note, testicular removal made a rooster into a capon which was much more palatable. The other common presentation of endocrine disease was thirst, copious production of urine and weight loss. Descriptions of this condition can be seen in medical literature from Egyptian papyri, and from Indian, Chinese, Greek and Arab sources. In the second Century AD, Aretaeous of Cappadocia[1] coined the name ‘diabetes’ though it was not till the 17th Century that the English anatomist and physician, Thomas Willis added ‘mellitus’ to diabetes in view of the sweet nature of the urine produced.
It was, however, the emergence of anatomy and physiology as scientific disciplines that concentrated minds upon those tissues of the body which looked like glands or organs and had a rich blood supply yet had no ducts (blood-glands). [2]
A Thyroid Narrative
The other gland relatively accessible to the knife, particularly if enlarged, was the thyroid. The Chinese used burnt sponge and seaweed to treat goitre over many millennia. In 150 AD, Hippocrates and Plato recognised this treatment and thought that the thyroid gland lubricated the larynx. Thomas Wharton, anatomist in 1656, wrote

about the anatomy of the gland that he thought it was there to heat the larynx. He named it ‘thyroid’ after the ancient Greek shield with a similar pronunciation. In German, the thyroid is ‘die Schilddrüse’, the shield gland. Two other anatomists, from Holland Frederik Ruysch in the 17th, from Switzerland Albrecht Von Haller in the 18th Century and Thomas Wilkinson King who was

a physiologist in the early 19th Century Britain, each wondered whether the thyroid elaborated a secretion which was carried away by the veins.

Thyroid history in the 19th Century, however, was a tale of three streams which converged as knowledge of its function emerged. These streams were Iodine, Goitre and Cretinism/hypothyroidism.
In 1811, the French chemist Bernard Courtois was extracting soda from burnt seaweed because of a shortage of the usual woodash. He tried to clear the deposit on the bottom of his copper extraction vessels with sulphuric acid and immediately noticed an intense violet vapour which condensed in the form of crystals. By circuitous routes, the crystals eventually reached both the French chemist Joseph Louis Gay-Lussac and, with the permission of Napoleon, Sir Humphrey Davy.

Each chemist separately identified a new chemical element which they agreed to call “iode”, or iodine, from the Greek word for violet.
It is not clear why iodine then became the focus for the treatment of thyroid enlargement. Initially suggested by Dr William Prout in London, 1816[4], it was John Elliotson from St Thomas’ Hospital who used it for goitre in 1819. In 1820, the Swiss physician Jean Francois Coindet used a tincture of iodine more widely with initial success. His treatment was questioned and fell into disrepute when some individuals developed hyperthyroidism (Jod-Basedow syndrome). In 1825, David Scott used iodine to treat goitre in Assam, India and in 1831, the French chemist Jean-Baptiste Boussingault used iodised salt in present day Columbia for the same condition. In 1835, Caleb H Parry followed by Robert James Graves from Ireland described hyperthyroidism with

goitre and noted an ophthalmopathy. The German physician Karl Adolph von Basedow independently reported similar cases in 1840 and firmly linked hyperthyroidism with the associated ophthalmopathy. In 1851, the French physician Caspar-Adolphe Chatin discovered that certain goitrous areas of Europe were associated with a low environmental iodine. While the national scientific community in France remained sceptical about Chatin’s evidence, iodine prophylaxis for goitre began in earnest.
The History of Diabetes
In 1815, the French chemist Michel Eugene Chevreul in Paris showed that the sweet tasting substance in the urine of patients with diabetes was glucose. In 1848, Hermann Von Fehling, a German chemist, developed a qualitative test for glucose in urine but it was not until 1889 that the pancreas became implicated in diabetes. Oscar Minskowski and Joseph von Mering, both German and working at the University of Strasbourgh, showed that dogs in whom the pancreas was removed developed diabetes mellitus. In 1893, The Frenchman Edouard Hedon showed that grafting pancreatic tissue back into the animal prevented diabetes from occurring. Something being secreted by pancreatic tissue was important for the prevention of diabetes. In the same year, the French scientist Gustave-Edouard Laguesse wondered whether the islands of tissue left after pancreatic duct ligation that had been described in 1869 by the German pathologist Paul Langerhans, might just be the source of the substance that controlled glucose levels. The concept of internal secretion by that time was close.
Contributions from Physiology and Anatomy
In 1849, the German Physiologist Arnold Adolph Berthold performed a classic ‘endocrine’ experiment while studying maleness in chickens.

He took 6 male chickens,castrated 4 and left 2 to develop rooster characteristics such as combs and wattles. Two castrati became chicken eunuchs or capons with soft flesh. In the final two, he transplanted the testes back into the abdominal cavity and found they developed normally as roosters. He concluded erroneously that the testes conditioned the blood to result in normal development. It was not until 1935 that pure testosterone was isolated.
In 1850, Thomas Blizzard Curling correlated the absence of thyroid tissue at autopsy in two children with cretinism. Come 1855, when physiological conundrums attracted the brightest of minds, the French physiologist Claude Bernard hypothesised that the liver might somehow secrete glucose into the blood while in the same year, Thomas Addison, an Edinburgh graduate working in Guy’s Hospital, proved, by autopsy, that suprarenal

gland destruction was present in 11 cases with weakness, vomiting and skin pigmentation which he understood to indicate chronic adrenal insufficiency but he was not believed at the time. In 1871, Charles Hilton Fagge presented a paper describing four children with sporadic cretinism and wondered whether the thyroid had ‘wasted’. Two years later in 1873, William Gull of Guys Hospital described hypothyroidism in adult life as creating a cretinoid appearance with a thick tongue. In 1877, William Ord described ‘mucous oedema’ and proposed the term ‘myxoedema’ for the adult condition. He also described the ‘practical annihilation’ of the thyroid gland at autopsy in these patients.
A Surgical Contribution

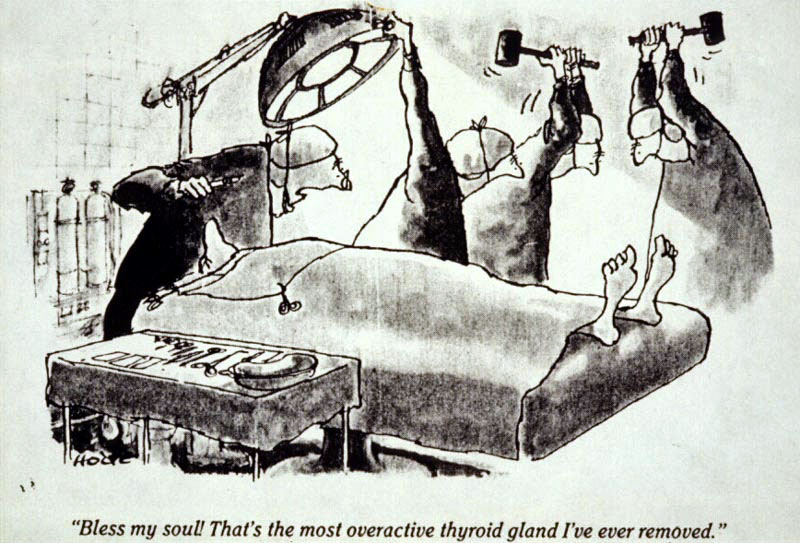
In 1882, Jaques-Louis Reverdin from Geneva and in 1883, Emil Theodor Kocher from Berne, both Swiss surgeons, noted that after total thyroidectomy, myxoedema was common. Because of this, they each experimented by conserving part of the gland during thyroidectomy, and no further cases of myxoedema occurred. [5] Although they did not understand what was happening, these surgeons had provided the medical community with the key to understanding the importance of the thyroid gland. Kocher went on to be awarded the NOBEL prize for medicine in 1909 for work relating to the surgical and medical treatment of thyroid disease.
In 1883, Felix Semon, a trainee laryngologist, later Sir Felix, suggested, to much ridicule from medical colleagues, that myxoedema and cretinism were one and the same condition, namely the effects of hypothyroidism. What he managed to do was to encourage his surgical colleagues to survey the experience of thyroid surgeons Europewide. Reporting in 1888 and using experimental work on thyroidectomised

monkeys by Sir Victor Horsley [6], the renowned scientist/surgeon who followed on in neurosurgery from Sir William Macewan, the report vindicated Semon and concluded that myxoedema was almost certainly due to loss of thyroid function and could lead to cretinoid features. Horsley went on to advocate surgical grafting of sheep thyroid into patients with myxoedema and in 1890, Bettencourt and Serrano of Lisbon had success with resolution of some clinical features in a case grafted under the breast. They then tried hypodermic injections of thyroid juice in 1891 and reported these beneficial too. The function of thyroid was now clear though the mechanism remained a mystery.
In 1891, Horsely and Professor George Redmayne Murray also continued along these therapeutic lines and

and used hypodermic injections of sheep thyroid extract into a patient with myxoedema and described a dramatic improvement. Murray provided details of his method of preparation and administration of the extract. Later that year, after publications from H W MacKenzie and E L Fox who had separately treated hypothyroid patients with thyroid extract by mouth, he changed to oral administration of pooled sheep thyroid extract with similar effect and so oral replacement therapy for glandular hypofunction was born.
Parathyroids, Pituitary and Adrenal
Ivar Sandstrőm, Uppsala medical student in 1887, confirmed the existence of the parathyroid glands in 50 autopsies and in 1901, the French physiologist Eugene Gley linked the absence of parathyroids after thyroid surgery to tetany which was often a sequel. [9]
Although the pituitary gland had been recognised in previous years at autopsy, for instance in studies of the two Irish Giants, its clinical role was more difficult to define because of its position in the centre of the skull. Clinical interest in the pituitary gland mainly arose from the studies and description of Acromegaly by Drs Pierre Marie, French neurologist, and José Dantas de Souza-Leites from Brazil in 1886 [10].
In 1893, George Oliver was interested in extract of adrenal gland to treat low blood pressure. He listed the help of Edward Shafer, Professor of Physiology at University College, London and found that his extract greatly raised the blood pressure in dogs. They both went on to discover that the effect was due to extract of medulla and not cortex.
Clearly, the important parts of the ‘endocrine’ or blood-gland jigsaw were gradually being assembled and one-by-one, the glandular origins of clinical deficiency syndromes were becoming clearer. The work on insulin, in particular, clearly pointed to a pancreatic source for a secretion of some sort preventing diabetes.
The Fog Clears
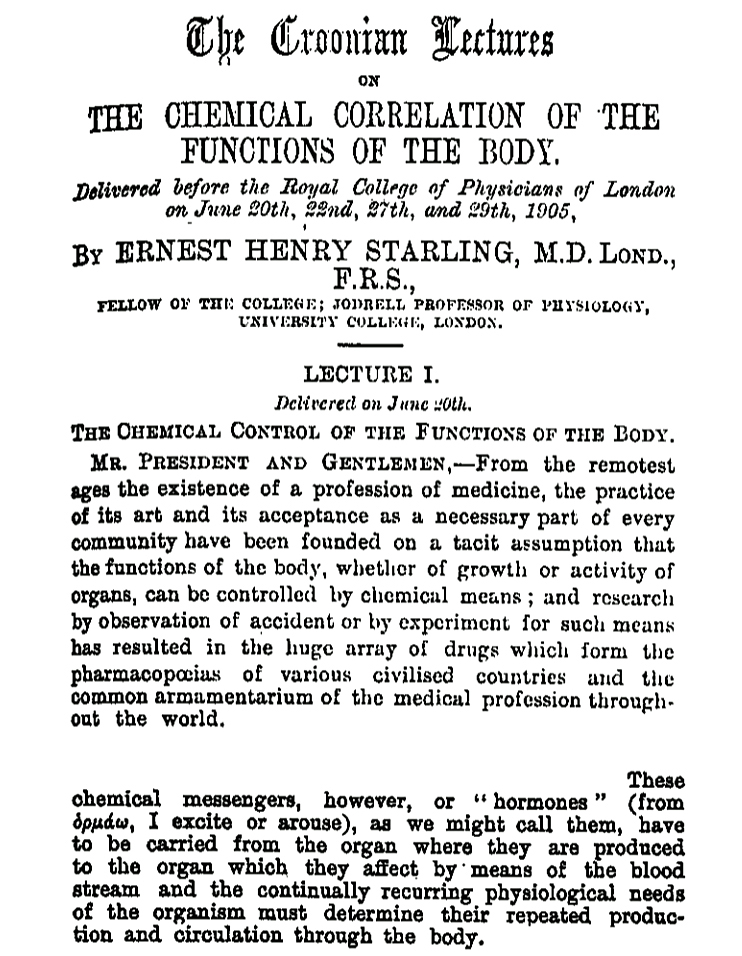
In 1905, the British physiologists Ernest Starling and his brother-in-law William Bayliss discovered something in the blood that caused the pancreas to secrete digestive juices.

Their experiment was in two parts. Firstly, they had used a completely denervated loop of duodenum, activated it by food, and found it stimulated pancreatic juice flow. Thinking that it must be something in duodenum, they liquified duodenal mucosa, injected it into the denervated animal model and found again that pancreatic juice flowed. Starling and Bayliss realised that a substance, which they called ‘secretin’, passed from the stimulated duodenum to the pancreas to stimulate it by virtue of the circulation of blood and not by the nervous system. They confirmed this hypothesis on the second experiment. Starling proposed after consultation with a classics trained colleague that such substances were called ‘hormones’ after the Greek ‘ormao’ – to excite, and at this precise point in history, a new speciality called ‘endocrinology‘ emerged. It studied substances produced by one tissue and then transported by the circulation of blood to another tissue, called the target.
The final part of the jigsaw, the concept of circulating hormones, had fallen into place in the early 20th century. The work by Frederick Grant Banting, Charles Best, John J R MacLeod and James Collip in extracting an insulin soup from atrophied pancreatic glands, purifying it, and by 1921, using the purified material in clinical practice was a monumental moment in the history of endocrinology. They had learned the lessons of the past and even had a name for the substance because in 1909, the Belgian physician Jean de Mayer had named the putative substance produced by the Islets of Langerhans, “insulin”.
When supplies of the purified animal sourced insulin reached the UK in May 1923, they saved the life of Dr Robert (Robin) Daniel Lawrence, a Scot from Aberdeen, among many others. Lawrence became one of the first UK physicians in diabetes at King’s College Hospital, London. He later co-founded the Diabetic Association with author and historian Herbert George (H G) Wells which later became the British Diabetic Association.
Although physiologists and the new ‘endocrinologists’ were unable to directly quantitate the actual hormones at this time, indirect ways were devised by them and physiologists to measure the ‘exciting’ effects of hormones on other tissues. It would be another 40 years before clinical measurement of insulin in blood would be possible but at least in 1921, there was a rational treatment for diabetes and myxoedema.
References
[1]. Milestones in the history of diabetes mellitus: The main contributors. World Journal of Diabetes, 2016, Jan 10; 7 (1): 1-7.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4707300/
[2] Starling Review: Ernest Starling and ‘Hormones’: An historical commentary, by John Henderson. Journal of Endocrinology, Volume 184, Issue 1, 2005, pages 5-10.
http://ressources.unisciel.fr/biocell/chap11/res/03_hormone_starling_henderson.pdf
[3] By courtesy of the European Thyroid Association and from the 4th Annual Meeting in Berne, 1971, President Prof H. Studer.
[4] A History of Iodine Deficiency Disorder Eradication Efforts, by J Woody Sistrunk and Frits van der Haar, in ‘Iodine Deficiency Disorders and Their Elimination’, Editor Elizabeth N Pearce, Associate Professor of Medicine, Boston University School of Medicine, Boston, MA, Springer 2017. Accessed on 12 February, 2018.
[5] Hypothyroidism and Thyroid Substitution: Historical Aspects by J Lindholm and P Laurberg, 2011. Journal of Thyroid Research, Volume 2011, Article ID809341. Accessed 12th February, 2018.
http://hindawi.com/journals/jtr/2011/809341/
[6] The Discovery of Thyroid Replacement Therapy. JLL Bulletin: Commentaries on the History of Treatment Evaluation. Stephan D Slater, 2010. Accessed 20 November 2017.
jameslindlibrary.org/articles/the-discovery-of-thyroid-replacement-therapy/
[7]. In. ‘Sir Victor Horsely, an inspiration’. BMJ. 2006; 333, 1317.
[8]. By courtesy of The James Lind Library.
[9] The History of Parathyroids. Accessed 20th November, 2017.
http://endocrinesurgeon.co.uk/index.php/the-history-of-the-parathyroids
[10] In the land of Giants: the legacy of Jose Dantas de Souza Leite. Accessed 20 November, 2017.
http://scielo.br/pdf/anp/v73n7/0004-282X-anp-73-7-0630
H W Gray
J A Thomson